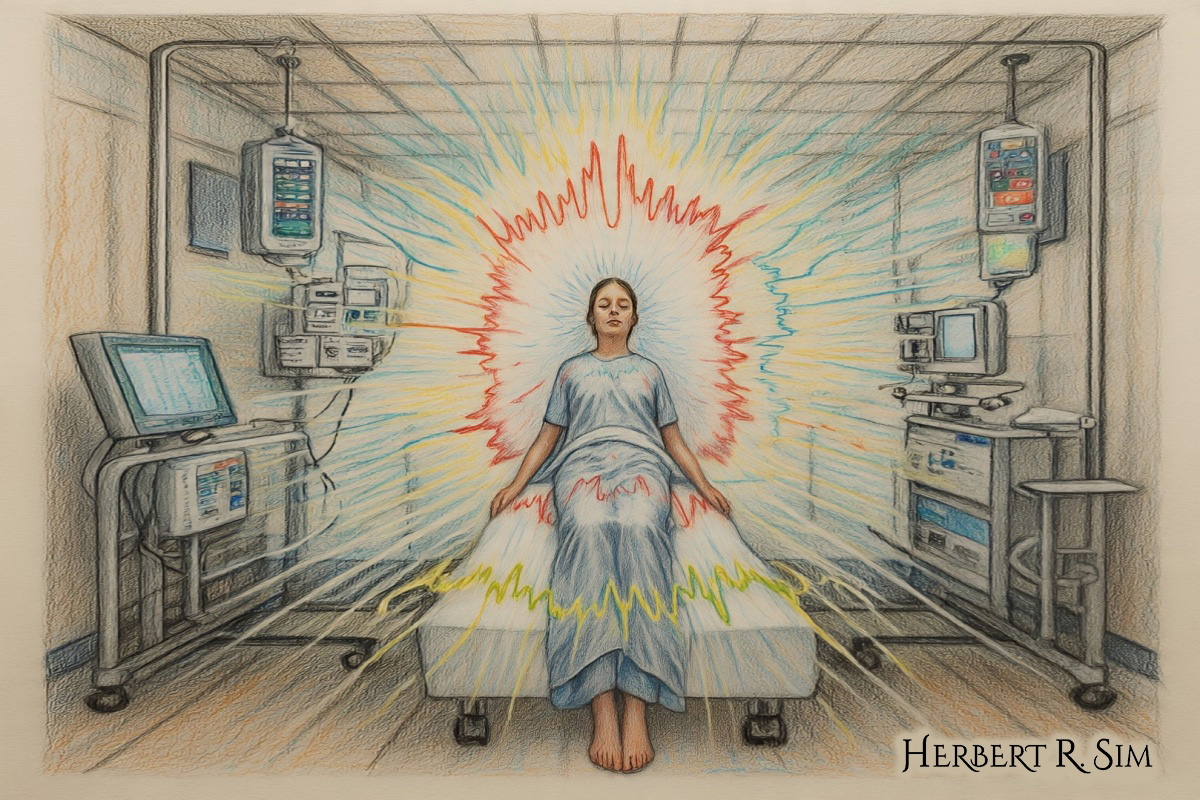
Above is my illustration featuring the neuroscience behind Near-Death Experiences (NDEs).
Near-death experiences — reports of leaving one’s body, moving through a tunnel, encountering an all-enveloping light, or reliving a “life review” — are strikingly consistent across cultures and eras.
Prospective and retrospective studies suggest they’re not rare: among people resuscitated after cardiac arrest, roughly one in ten to one in five report NDE-like memories once they recover.
That prevalence, plus the vividness and long-lasting psychological impact of these experiences, makes them an important (and now tractable) target for brain science.
What exactly do people report—and what brain systems can generate it?
Some of the best-mapped NDE elements are the out-of-body experience (OBE) and the sense of watching oneself from above. Two decades of lesion mapping and direct brain stimulation point to the temporo-parietal junction (TPJ) — especially the angular gyrus—as a key multisensory hub where vision, vestibular information (balance/acceleration), and proprioception are bound into a coherent “where am I?” model.
When that binding is disrupted, the self can seem to “float” away from the body. Seminal case work showed that stimulating the right angular gyrus could repeatedly evoke OBE-like sensations in a conscious patient. Larger neurological series linked autoscopic phenomena (seeing one’s own body) to TPJ dysfunction.
Follow-up neuroimaging and neuropsychological work extended this into a broader model: the TPJ appears to mediate spatial unity between self and body, so perturbations there (by seizures, electrical stimulation, or mismatched sensory information) can produce illusory self-location and perspective shifts — core ingredients of OBEs that often appear within NDEs.
This framework has even been echoed in human stories: reporting on recent clinical stimulation studies of the anterior precuneus — another hub nestled near the brain’s “default mode” midline — describes reproducible sensations of weightlessness, falling, or detachment that resonate with OBE descriptions.
Hypoxia, CO₂, and the “tunnel”
Physiology matters. In crises that precipitate NDEs — cardiac arrest, major blood loss, suffocation—the brain is starved of oxygen and blood flow while carbon dioxide rises. Classic work on altitude exposure, anesthesia mishaps, and cardiac arrest implicates hypercapnia (high CO₂) and hypoxia in producing visual and vestibular distortions, sometimes including the famous “tunnel of light.”
Early clinical studies even found that higher CO₂ during resuscitation correlated with NDE reports, pointing to a plausible mechanistic driver for visual narrowing and bright lights as retinal and cortical circuits falter.
Life review, time distortion, and memory systems
A dramatic “life review” is one of the most memorable motifs. While it’s impossible to replay someone’s mind on demand, rare recordings around death and new bedside studies now let us ask whether known memory networks are active.
A much-discussed case report captured an 87-year-old patient’s electroencephalogram as he died unexpectedly in the scanner, showing coordinated shifts in rhythms (including gamma) around the moment of cardiac arrest. Those patterns overlapped with states tied to memory recall and dreaming, offering a tantalizing, if preliminary, physiological bridge to “life flashes.” Subsequent ICU studies in humans extend that theme.
Why are we talking about gamma?
In 2013, a landmark animal study observed a surge in high-frequency (gamma) activity and increased inter-area connectivity in rats immediately after cardiac arrest — despite the cessation of heartbeat. The effect resembled patterns often associated (controversially) with conscious processing. A 2023 study then captured analogous gamma-coupled activity in two of four dying ICU patients after withdrawal of life support, particularly over regions implicated in vivid experience. Science’s news coverage put it plainly: a dying brain can transiently show a coordinated “last surge.” Together, these findings suggest the end-of-life brain is not simply flickering out—it may briefly enter a paradoxically organized state.
Case evidence adds texture. In a widely discussed bedside report from 2022, clinicians monitoring an older patient who later died observed coordinated gamma-range dynamics surrounding cardiac arrest. University of Michigan investigators have also publicized converging patient data, emphasizing that while awareness cannot be inferred from rhythms alone, the physiology is compatible with reports of vivid inner experience.
Are NDE memories “realer than real”?
The most ambitious effort to probe NDEs during resuscitation is AWARE-II, a 25-site study that combined EEG, oxygenation monitoring, and hidden audio-visual targets in rooms where cardiac arrests occurred.
Among survivors available for interview, about one-fifth described a structured “recalled experience of death,” and investigators recorded brain activity consistent with organized processing during CPR in some cases. Media coverage highlighted the paradox: seemingly lucid, structured memories can emerge from patients who, from the outside, appear unresponsive.
Sleep physiology, migraine, and the brain’s “brakes”
Another thread links NDE proneness to sleep-wake boundary phenomena. In clinic and population studies, people who experience REM intrusion — dreamlike imagery or paralysis “spilling” into wakefulness — report NDE-like experiences more often.
A classic case-control study in Neurology proposed this REM instability as one substrate; a large online study replicated an association; and recent neurology work suggests overlap with migraine mechanisms. Under extreme stress, the brain’s normal inhibitory “brakes” can fail, disinhibiting imagery, emotion, and perspective shifts — exactly the ingredients NDEs capture.
Syncope, shutdown, and the moment the lights dim
Transient loss of consciousness (syncope) can produce narrowed vision, tunnel effects, and dreamlike scenes. Modern EEG studies of syncope hint at a rapid sequence: cortical slowing, disconnection, then rebound activity. Those spectral signatures are consistent with subjective “fade to black” and brief, vivid imagery—a useful lab proxy for some NDE elements that occur when blood flow drops abruptly.
A neuroscientific framework is taking shape
Recent theoretical work argues that NDEs are a unique window into “disconnected consciousness” — highly structured experience when normal sensory inputs and outputs are compromised.
Integrating models of consciousness (global neuronal workspace, posterior “hot zone,” and predictive processing), authors propose that extreme physiology can yield transient pockets of coordinated cortical activity, heavily shaped by memory and expectation, even when outward behavior is nil.
A 2024 anesthesiology review synthesizes this emerging picture, asking how to monitor, mitigate, or even therapeutically engage with end-of-life consciousness.
Not just metaphors: lessons from engineered illusions
If mismatched sensory evidence can unbind the self, technologies that deliberately produce those mismatches should evoke similar phenomena — and they do.
Virtual-reality experiments that manipulate embodiment and perspective can induce out-of-body sensations and presence illusions in healthy participants, demonstrating how malleable our embodied self-model is under the right conditions.
That malleability helps demystify why OBEs can arise during crises that disrupt normal multisensory integration.
Clinical implications
For critical-care teams, NDEs are not curiosities. A prospective ICU study across illnesses (not just cardiac arrest) found that about 15% of survivors reported NDE-consistent memories and that these experiences shaped quality of life months later — highlighting the need to ask about them and to support patients who report distressing versions.
Meanwhile, anesthesiologists have documented unexpected changes on processed EEG around withdrawal of life support and in organ-donation contexts, raising questions about comfort measures and communication with families at the end of life.
Where the line is—and isn’t
There’s a danger in over-interpreting the data. Gamma oscillations and network “coupling” aren’t synonymous with conscious awareness, and small samples near death limit strong conclusions. Still, careful reporting has emphasized how the new findings challenge simplistic shutdown narratives and invite better monitoring.
A widely read feature captured the growing consensus among researchers: something organized can happen in the dying brain, and understanding it could improve resuscitation and end-of-life care.
So what is an NDE, in brain terms?
Pulling these strands together suggests a convergent model:
- Triggering physiology: abrupt hypoxia, hypercapnia, and blood-flow changes destabilize neural circuits. In some individuals (especially with REM intrusion propensity or migraine), the brain’s usual inhibitory “brakes” loosen. Sensory mismatch at hubs like the TPJ uncouples the self from the body’s coordinates, yielding OBEs.
- Network dynamics: paradoxical bursts of coordinated, high-frequency activity — and transient increases in inter-areal connectivity — can arise as systems fail, potentially supporting brief windows of vivid, internally generated experience while the outside world sees no response.
- Content construction: the “life review,” lights, presence, and profound calm draw on memory/emotion systems and predictive models shaped by culture and expectation. Rare recordings and case studies fit with activation of networks used in dream recall and autobiographical memory.
- Aftereffects: many experiencers report lasting shifts in attitudes and values. Prospective studies and follow-ups in ICU survivors underscore both salutary and distressing trajectories, arguing for routine screening and support in survivorship clinics.
None of this “explains away” the meaning people attach to their experiences. Rather, it explains how such experiences become possible in a brain under extreme duress—and why their features cluster the way they do.
Where research is heading
Expect three near-term advances.
- Richer bedside monitoring—multi-channel EEG, cerebral oximetry, and blood-flow ultrasound — during resuscitation will clarify when and for how long organized dynamics persist.
- Carefully controlled comparisons between NDE narratives and psychedelic states (ketamine, DMT, psilocybin) are already quantifying overlaps and differences in content and network signatures, helping to separate what is specific to dying physiology from more general routes to “disconnected consciousness.”
- Ethically constrained stimulation studies (e.g., intraoperative mapping) will continue to reveal the causal role of TPJ and midline structures in self-location and presence — the mechanistic heart of out-of-body phenomena.
Bottom line
NDEs aren’t evidence that brains do nothing as bodies fail. If anything, the latest work shows the opposite: under extreme threat, the brain can enter a fleeting, highly organized mode that stitches together bodily maps, memories, expectations, and emotion into a coherent narrative — one that feels “realer than real,” even when it’s constructed in the dark.
For neuroscience, NDEs have gone from taboo to testable. As methods get better — and as clinicians treat them as part of survivorship—these extraordinary experiences are poised to teach us something ordinary but profound: how brains make selves, even at the edge of life.
